* Brain Mapping for Stroke and MS
* Neuropsychological Test
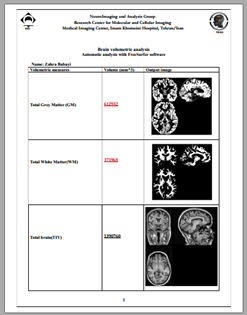
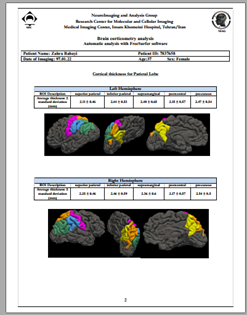
Brain metabolic imaging (MRS)
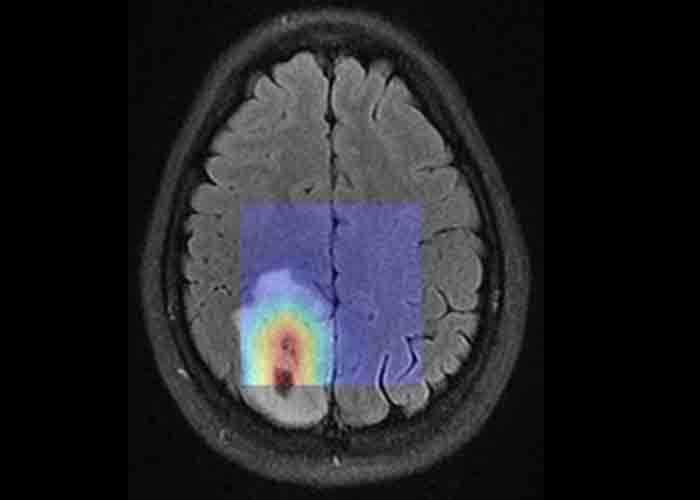
The purpose of brain metabolic imaging, specifically Magnetic Resonance Spectroscopy (MRS), is to ascertain the characteristics of brain damage. This advanced imaging technique provides valuable insights into the biochemical and metabolic profile of the specific target tissue being examined.
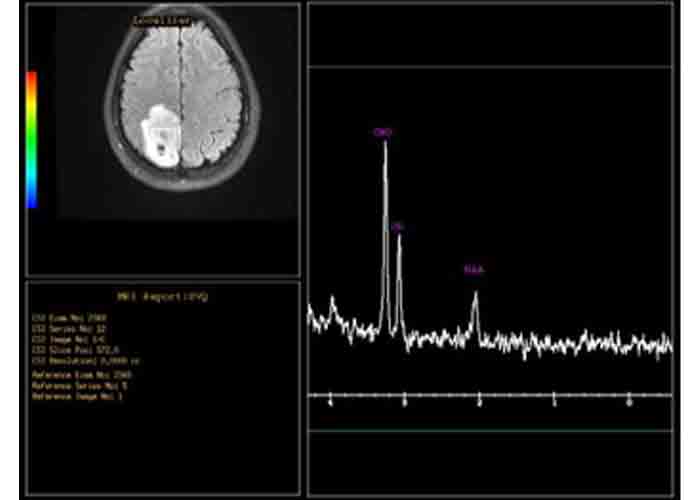
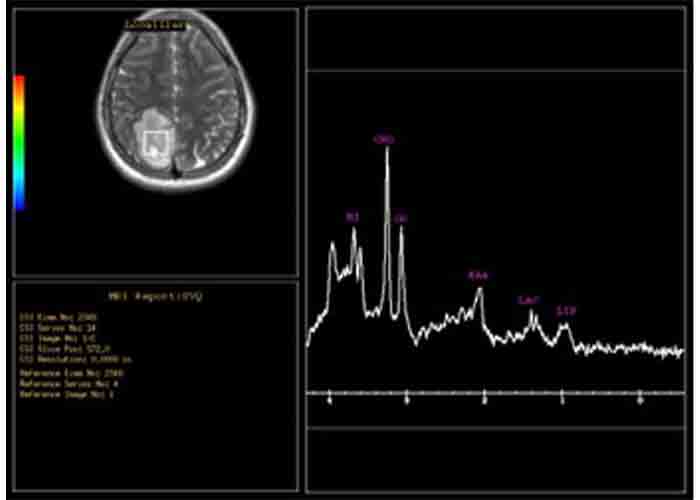
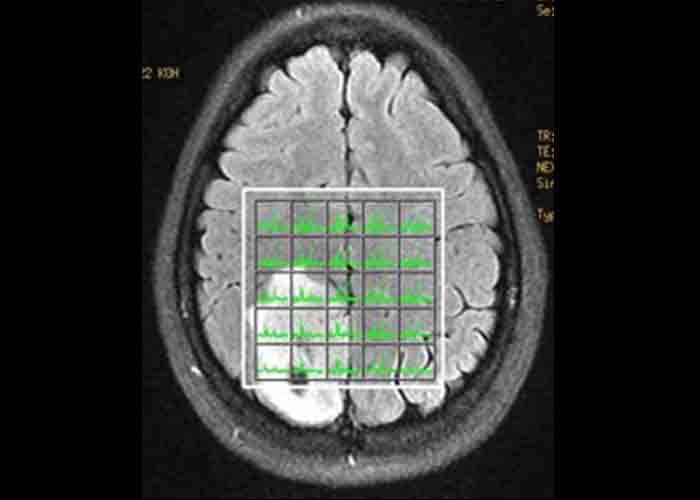
Top row: An illustrative instance of single-voxel Magnetic Resonance Spectroscopy (MRS) conducted with echo times of 144 ms (right) and 35 ms (left).
Bottom row: Multi-voxel MRS (right) and the corresponding metabolic map derived from the identical lesion.
In which scenarios are they indicated:
- Determination of the specific type of brain tumors.
- Discrimination between tumors and other lesions, such as Multiple Sclerosis (MS) plaques, abscesses, and inflammatory conditions.
- Presurgical planning prior to brain surgery.
Assessment of treatment options for brain and nerve diseases, including brain surgery, brain radiotherapy, and chemotherapy.
- Diagnosis of tumor recurrence following completion of radiotherapy.
Creating a metabolic map of the tumor and its adjacent regions prior to surgery and radiotherapy assists physicians in determining the most suitable treatment approach for patients.
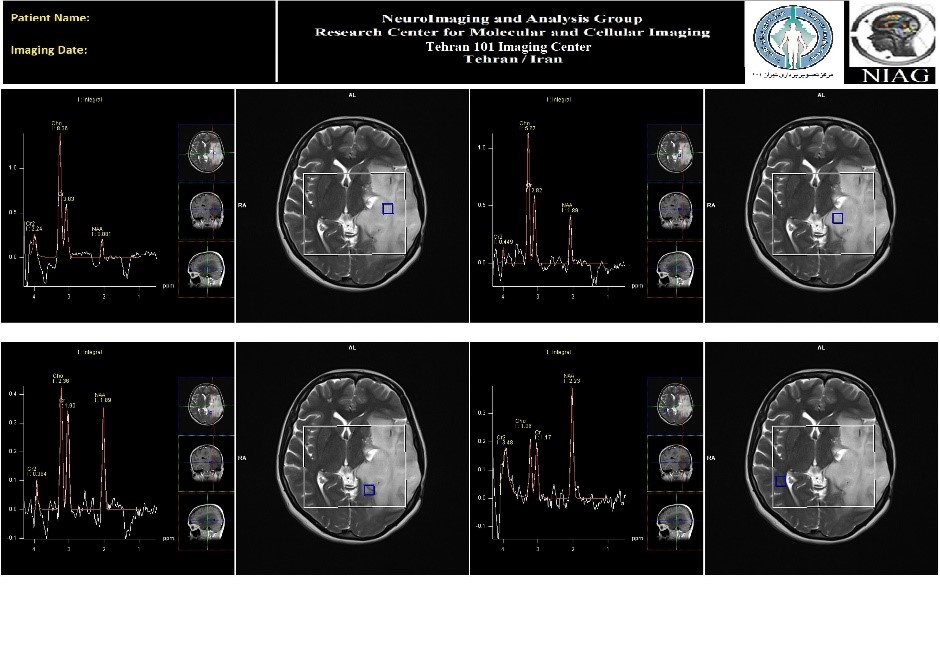
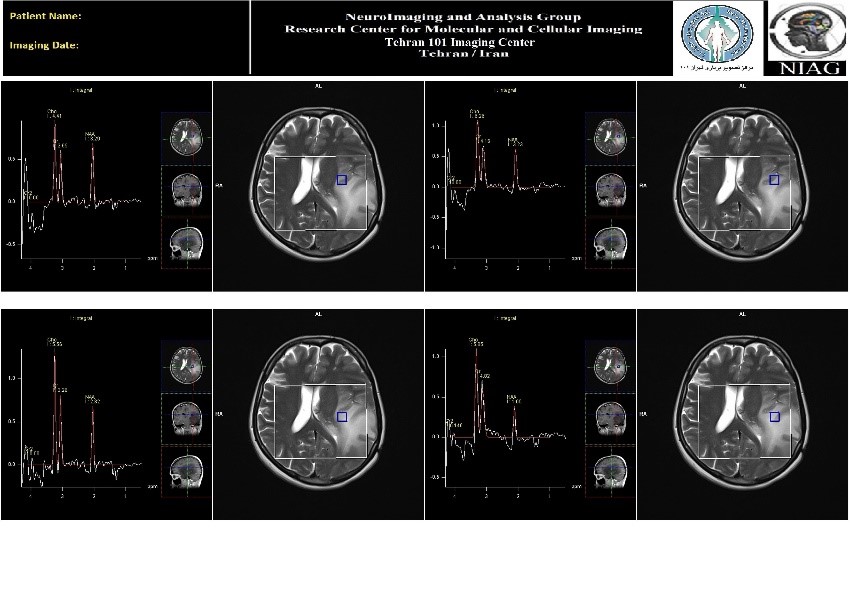
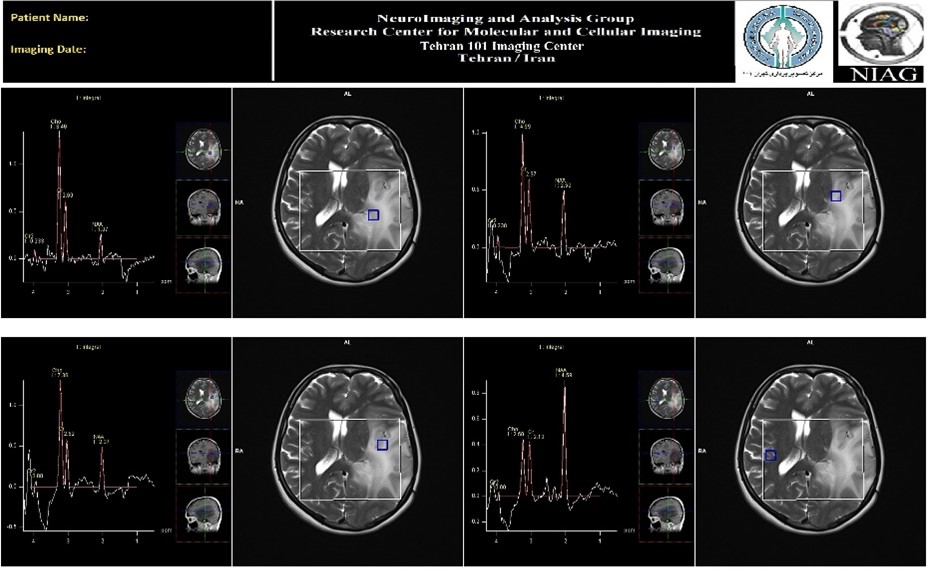
An illustrative instance of 3D Magnetic Resonance Spectroscopy (MRS) conducted within the NIAG Brain Image Analysis Group.
Functional Magnetic Resonance Imaging (fMRI):
Functional brain Imaging, such as (fMRI), has advanced the field of medical imaging by enabling the investigation and recording of human brain activity in different regions. In addition to visualizing damaged tissues and structural changes in the brain, MRI can now capture the image of brain tissue activity.
During fMRI, the patient is asked to perform specific activities, such as hand movements or speech, while being imaged. This elicits an increase in neural activity within a particular brain area. For instance, the patient may be instructed to move their index finger or repeat a word. Such actions lead to changes in electrical activity and enhanced blood flow within the corresponding motor region of the brain. Consequently, the blood flow in the activated area increases compared to other regions, resulting in elevated blood oxygen concentration. Ultimately, these changes manifest as differences in the received signal intensity of the respective brain tissue, which can be quantified using an MRI machine.
Application of fMRI in brain surgeries:
Functional brain imaging, such as fMRI, has significant applications in the planning of brain surgeries. For instance, when a neurosurgeon aims to remove a tumor located in proximity to speech, movement, vision, or other functional centers of the patient's brain, they may request an fMRI to determine the distance between the tumor and each of these centers. These images serve as valuable guidance for the surgeon, enabling them to minimize the risk of damaging the areas associated with the activity of these centers during the surgical procedure.
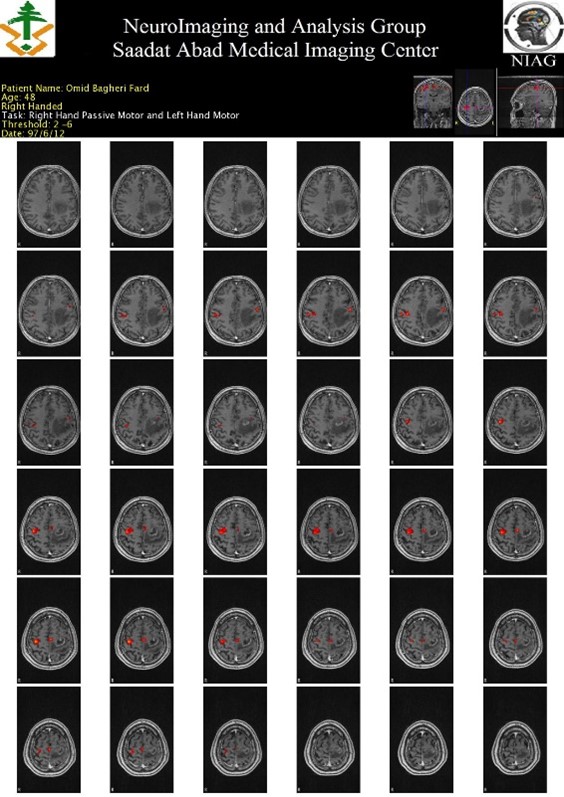
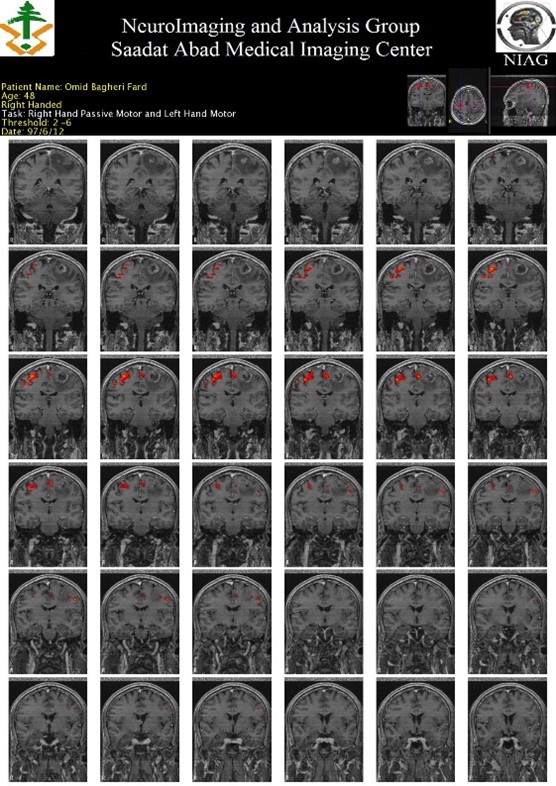
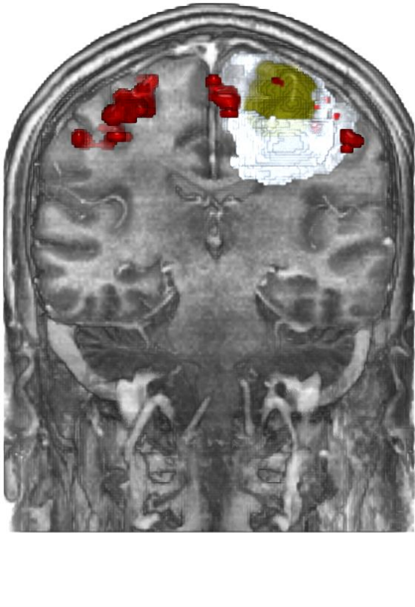
Top row: The fMRI data analysis reveals significant findings pertaining to a disease characterized by a lesion located in close proximity to the motor center responsible for right hand movements.
Bottom row: A 3D reconstruction depicts the tumor (highlighted in yellow), edema (depicted in white), and the areas of brain activity associated with the right hand (shown in red).
Tests available at the center include:
Speech tests: These tests aim to activate the speech motor centers (Broca's area) and speech sensory centers (Wernicke's area).
Motor tests: These tests are designed to assess the activity of motor centers responsible for hand, foot, lip, and tongue movements.
Memory tests: These tests are specifically designed to investigate the activity of the hippocampus, a region crucial for memory functions.
Vision test: This test is designed to evaluate the activity of the visual area located in the occipital lobe.
Hearing test: This test is conducted to assess the activity of areas associated with hearing and auditory comprehension.
Olfactory test: This test examines the activity of the olfactory centers involved in the sense of smell.
fMRI is requested in the following cases:
1. Presurgical planning: It is utilized to aid in the planning process before brain surgery.
2. Treatment design: It is employed in the design phase prior to invasive brain treatments, such as radiotherapy.
3. Diagnosis of brain and nerve diseases impacting human performance.
4. Diagnosis of behavioral disorders affecting human performance.
5. Assessment of diseases affecting language, memory, sensory perception, movement, hearing, vision, smell, behavior, or addiction.
6. Evaluation of treatment efficacy in psychotherapy, neurorehabilitation, neurological diseases, psychiatric treatments, and addiction.
7. Specialized or differential diagnoses that cannot be achieved through conventional imaging methods.
Prescription guidelines;
- Determining the type and location of the brain imaging areas that are required, as well as specifying the type of structural imaging in the prescription.
- Clearly stating the rationale for requesting specialized imaging in the prescription.
- Furthermore, the prescription should include a thorough history of the patient's disease and the main therapeutic interventions that have been taken, or any relevant forms available to the doctor. This ensures that the prescription is comprehensive and provides all necessary information for the appropriate imaging and treatment planning.
Nerve fiber imaging (tractography or diffusion tensor imaging (DTI)):
Brain function relies on an intricate network of nerve fibers that connect various regions of the brain. Specialized diffusion tensor imaging, known as DTI, utilizes the movement of water molecules along these fiber tracts, mirroring the transmission of nerve impulses. This imaging technique enables the visualization of these neural structures. DTI not only provides insights into the neural pathways but also proves valuable in describing and diagnosing disorders of the brain's white matter, such as space-occupying tumors, stroke, and epilepsy. Furthermore, in surgical cases, the mapping of crucial nerve fibers, along with their proximity and distance from the target tumor, aids in enhancing the precision and accuracy of the procedure.
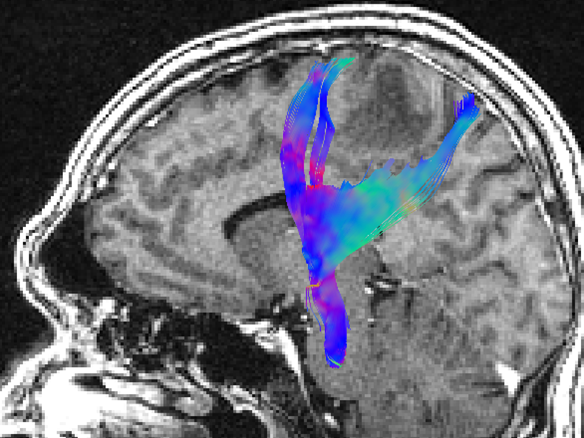
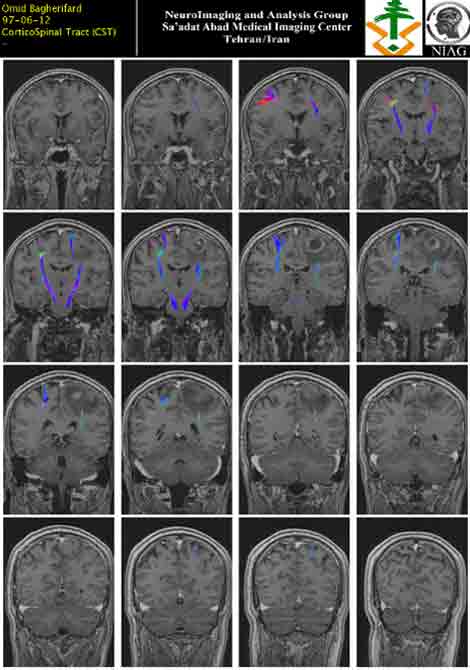
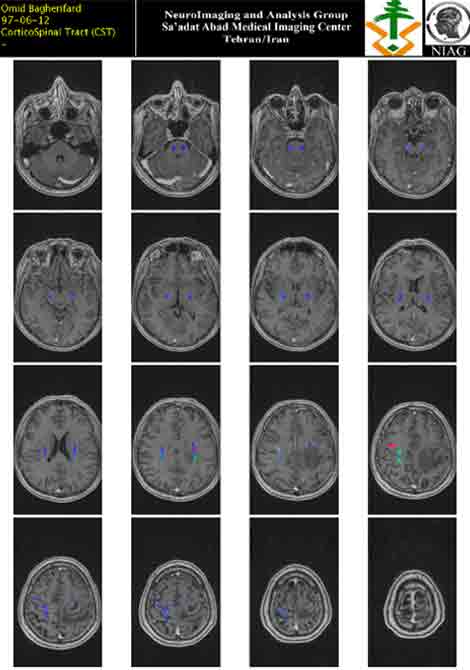
The above provided images depict the results of DTI imaging analysis, specifically the reconstruction of motor fiber pathways .
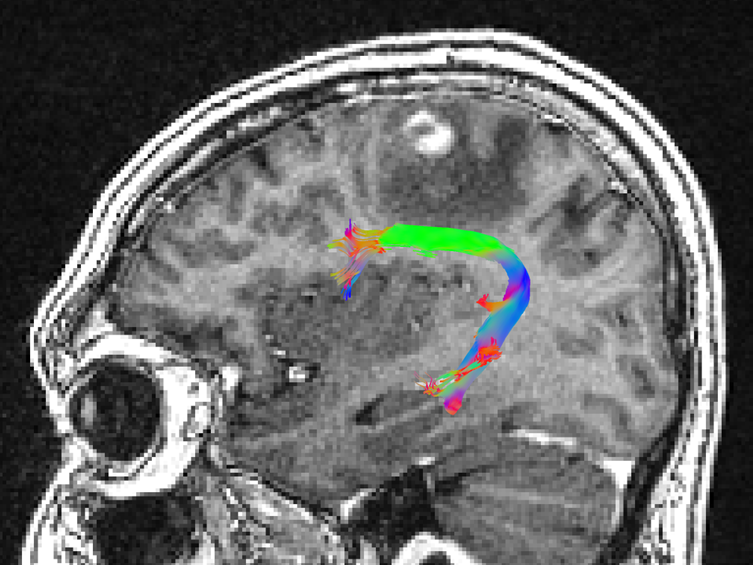
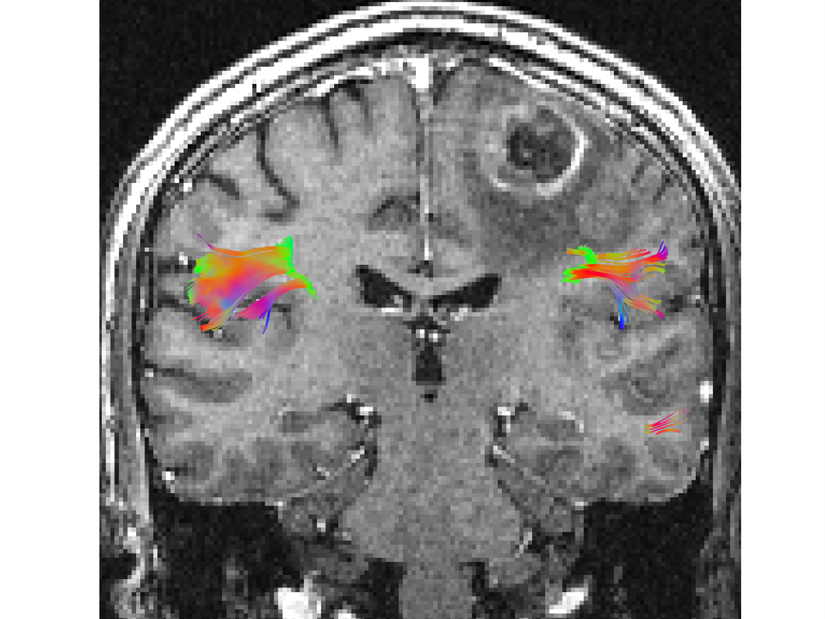
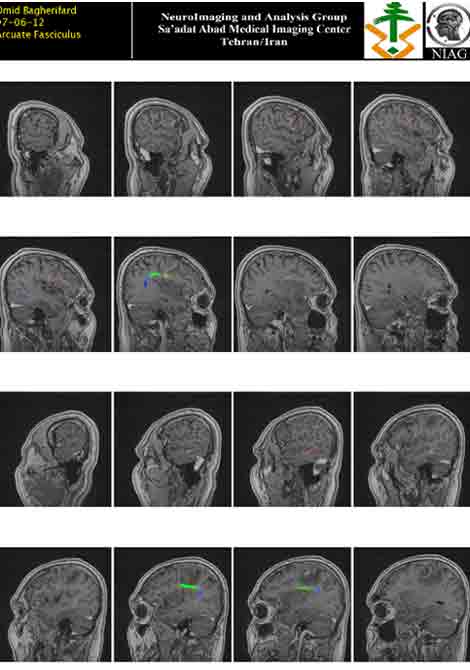
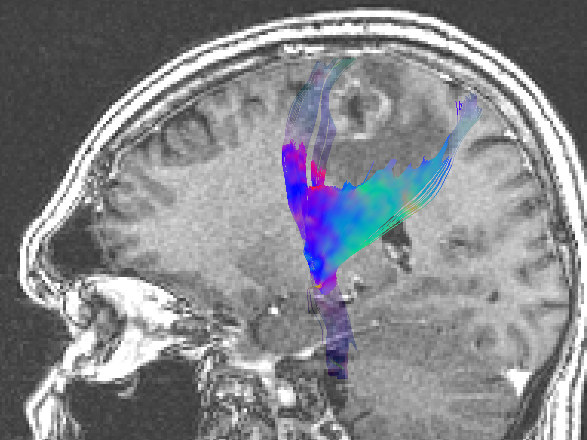
The above provided image showcases the reconstruction of speech pathway fibers.
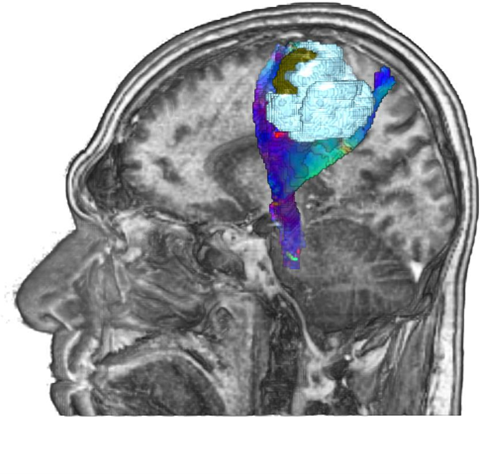
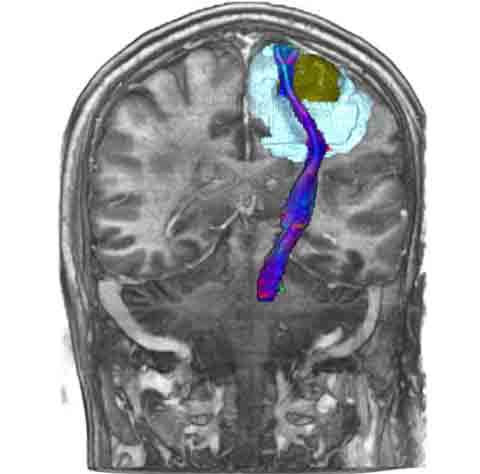
The accompanying image displays a 3D reconstruction of a tumor (highlighted in yellow), edema (indicated in blue), and motor fibers located in close proximity to the lesion.
Neural pathways that can be analyzed are as follows:
- Motor pathways, such as the corticospinal fibers, which are responsible for coordinating voluntary movements.
- Language pathways, including the Arcuate fibers, IFOF (Inferior Fronto-Occipital Fasciculus), Uncinate fasciculus, SLF (Superior Longitudinal Fasciculus), and ILF (Inferior Longitudinal Fasciculus), which are involved in speech production and comprehension.
- Memory pathways, such as the fornix fibers, which play a role in memory formation and retrieval.
- Visual pathways, which comprise the optic nerve, optic tract, and optic radiation, and are responsible for transmitting visual information from the eyes to the brain.
- Olfactory pathways, involving olfactory nerve fibers, which enable the perception of smell.
- Brainstem fibers, like the MLF (Medial Longitudinal Fasciculus), are involved in coordinating eye movements and maintaining balance.
- Cerebellar pathways, such as cerebellar connections, contribute to motor control, coordination, and balance.
For which clinical scenarios is DTI imaging typically requested?
1. Presurgical planning prior to brain surgery.
- Planning before invasive brain treatments, such as radiotherapy.
3. Diagnosis of brain and nerve diseases that have impacted the structure of brain fibers.
4. Specialized or differential diagnoses that cannot be achieved with conventional imaging methods.
Prescription guidelines;
1. Specify the specific type of fiber or tract and the precise location of the brain imaging areas required, or indicate the type of structural imaging necessary in the prescription.
2. Clearly state the reason for requesting DTI imaging in the prescription.
3. Provide a comprehensive medical history of the patient, including relevant therapeutic interventions, in the prescription or accompanying forms available to the physician.
Perfusion brain imaging:
Perfusion brain imaging refers to the physiological assessment of the brain using a combination of structural and functional imaging techniques conducted on an MRI machine operating at either 1.5T or 3T. Initially, raw and primary images are acquired using perfusion protocols based on T1 for Dynamic Contrast Enhanced (DCE) calculations or based on T2 for Dynamic Susceptibility Contrast (DSC) calculations. These protocols are executed using specialized imaging devices that facilitate the necessary processing and calculations. If further quantitative analysis and calculations are required beyond the capabilities of the imaging device, the images and signals are transferred to high-performance personal computers equipped with software capable of spectrum information analysis and quantification (such as PMA). It is crucial to ensure qualitative correction, measurement, and validation of the obtained information, which should be incorporated into statistical analyses. Various perfusion maps are generated and superimposed onto standard anatomical images, with the resulting images printed in color. Perfusion images and maps are primarily utilized for differential diagnoses that cannot be accomplished through conventional MRI imaging, focusing on lesion sites, their surrounding areas, and corresponding healthy tissue.
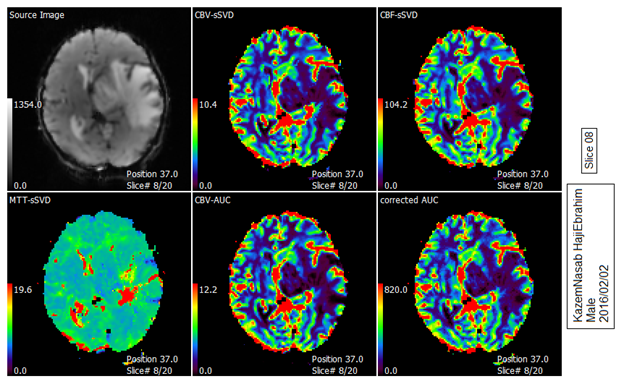
The provided photo depicts a perfusion map showcasing various parameters derived from the analysis of Dynamic Susceptibility Contrast (DSC) images.
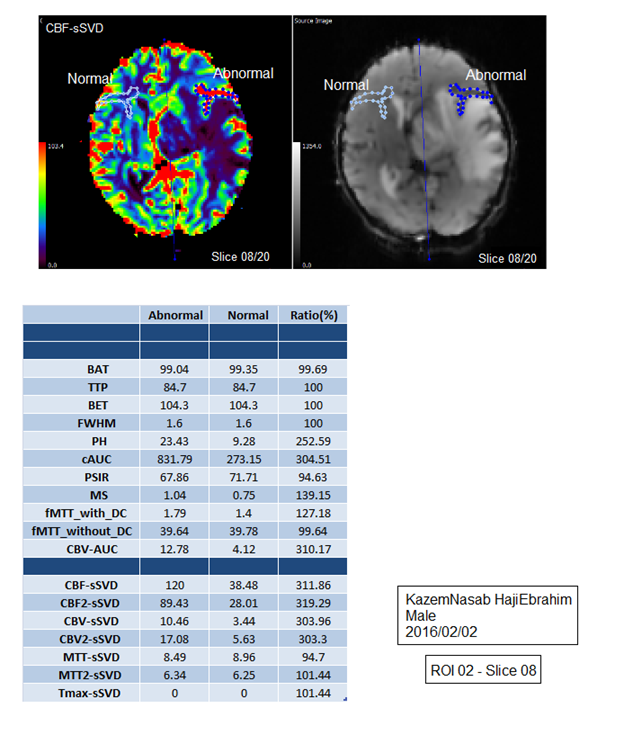
The above photo illustrates parameters measured within the abnormal area in terms of perfusion.
Brain tumor imaging (Tumor Mapping):
Brain tumor imaging, also known as Tumor Mapping, involves a comprehensive set of structural and physiological imaging techniques conducted using an MRI machine operating at either 1.5T or 3T. The process begins by acquiring raw and primary images using standard protocols, along with Magnetic Resonance Spectroscopy (MRS) or perfusion protocols, utilizing specialized imaging devices that incorporate the desired imaging protocol and facilitate necessary processing and calculations. If there is a requirement for quantitative analysis and calculations beyond the capabilities of the imaging device, the images and signals are transferred to high-performance personal computers equipped with software for data analysis and quantification. It is crucial to ensure the qualitative correction, measurement, and statistical validation of the acquired data. Various perfusion maps are then generated, superimposed onto standard anatomical images, and subsequently printed in color. MRS or perfusion images and maps, derived from the lesion sites, their surrounding regions, and corresponding healthy tissue, are employed to facilitate differential diagnoses that are not achievable through conventional MRI imaging alone. In general, Tumor Mapping encompasses multi-protocol brain imaging techniques, including protocols with and without contrast enhancement, Fluid-Attenuated Inversion Recovery (FLAIR) imaging, Diffusion-Weighted Imaging (DWI) with Apparent Diffusion Coefficient (ADC) mapping, and either MRS or Perfusion methods.
Precise indications for prescribing this service include the following::
(Precise indications for prescribing this service are based on evidence-based paraclinical and clinical criteria, as well as the consideration of the number of cases in which providing this service is deemed necessary for a particular patient).
1. Differential diagnosis of brain and nerve diseases, specifically distinguishing tumors from other conditions.
2. Evaluation of treatment efficacy for various interventions such as brain surgery, brain radiotherapy, and chemotherapy.
3. Determination of the type, characteristics, and grading of neurological brain tumors.
4. Preoperative planning for brain surgery.
- 5. Presurgical planning prior to invasive brain treatments, such as radiotherapy.
Prescription guidelines;
1. Specification of the type and location of brain imaging areas required, or the type of structural imaging needed, in the prescription.
2. Identification of the purpose for requesting specialized photography in the prescription.
3. Documentation of the patient's medical history and relevant therapeutic interventions in the prescription or available forms provided to the doctor.
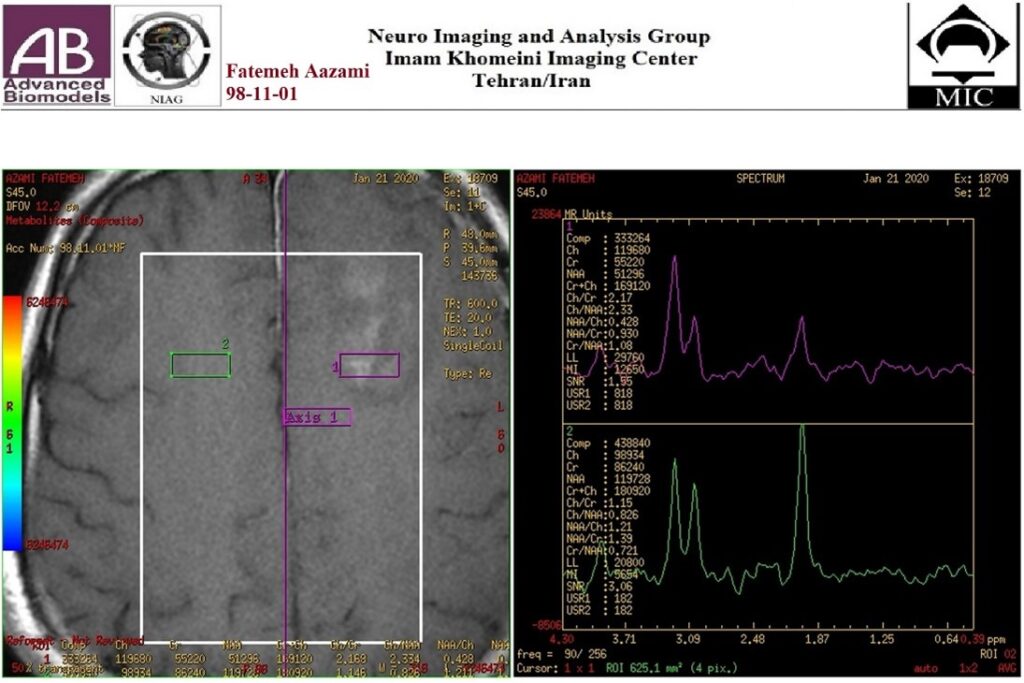
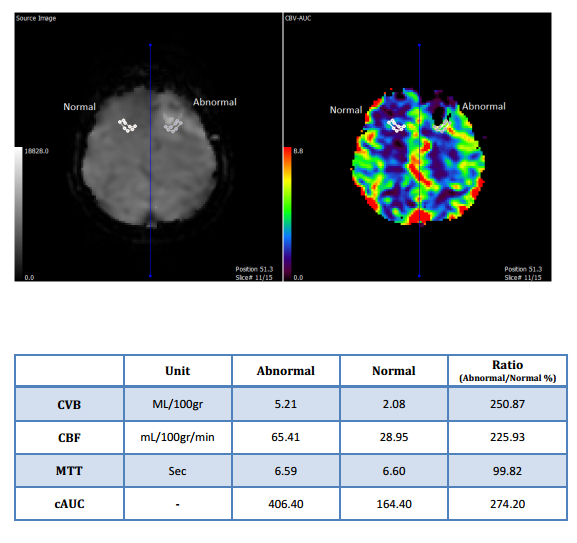
Image description: Analysis conducted for the Tumor Mapping protocol in a patient.
Seizure Mapping:
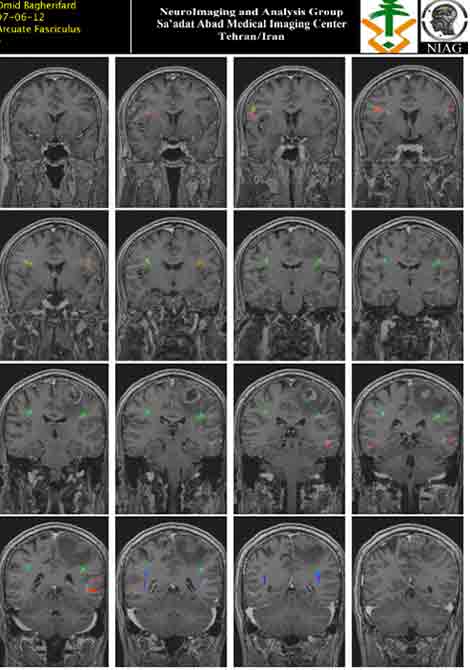
Seizure Mapping is a comprehensive imaging technique that involves the acquisition of structural, physiological, and metabolic data using an MRI machine operating at either 1.5 T or 3 T. Initially, raw and primary images are obtained utilizing standard, diffusion, and MRS protocols on devices equipped with the necessary imaging capabilities. Subsequent processing and calculations are performed by the imaging device. If quantitative analysis and calculations beyond the device's capabilities are required, the images and signals are transferred to powerful personal computers equipped with specialized software for information analysis and quantification. The obtained information is then qualitatively corrected, measured, and statistically validated. During Seizure Mapping, various perfusion maps are generated and superimposed on standard anatomical images, which can be printed in black and white or color. Comprehensive images and maps of the entire brain are acquired in three distinct orientations: coronal, axial, and sagittal. This multi-protocol brain imaging approach includes standard brain protocols, high-resolution structural imaging in three directions, T1 and T2 FLAIR sequences in at least two directions, Susceptibility-Weighted Imaging (SWI), contrast-enhanced imaging (if a lesion is suspected), diffusion tensor imaging (DTI) or Voxel-Based Morphometry (VBM) if feasible. Additionally, the evaluation encompasses the assessment of microstructural changes and Focal Cortical Dysplasia (FCD), as well as volume measurements to identify possible atrophy. In certain cases, involving underlying metabolic diseases or growth disorders, Chemical Shift Imaging (CSI) and Magnetic Resonance Spectroscopy (MRS) may also be employed.
Precise indications for prescribing this service include the following:
The precise indications for prescribing this service are determined by evidence-based paraclinical and clinical criteria. This service is indicated for the diagnosis of pathological factors or structural and physiological changes that contribute to the development of epilepsy.
- diagnosing pathological factors or structural and physiological changes that are the underlying cause of epilepsy.
- determining the type and extent of brain lesions that are responsible for causing epilepsy.
- Presurgical planning and preparation for invasive procedures aimed at treating epilepsy.
Prescription guidelines;
- Determining the type and location of the brain imaging areas that are required, as well as specifying the type of structural imaging in the prescription.
- Clearly stating the rationale for requesting specialized imaging in the prescription.
- Furthermore, the prescription should include a thorough history of the patient's disease and the main therapeutic interventions that have been taken, or any relevant forms available to the doctor. This ensures that the prescription is comprehensive and provides all necessary information for the appropriate imaging and treatment planning.
How can fMRI and DTI assist surgeons in their practice?
Neurosurgeons rely on Functional Magnetic Resonance Imaging (fMRI) and diffusion tensor imaging (DTI) to assist them in accurately planning surgical interventions for brain lesions, such as tumors. These advanced imaging techniques enable the surgeon to precisely determine the extent of the brain lesions in relation to important functional areas of the brain, including those associated with speech, vision, and motor control of the hands and feet. By utilizing fMRI and DTI, neurosurgeons can navigate and operate in a way that minimizes the risk of damaging critical functional areas, thus optimizing patient outcomes. Overall, this meticulous approach ensures the preservation of vital brain functions and enhances surgical outcomes.
The following services are provided within the group:
Designing tasks and protocols for functional magnetic resonance imaging (fMRI), as well as conducting imaging and analysis of fMRI images. This includes mapping and studying specific brain regions involved in various cognitive processes.
Capturing high-quality images and performing indepth analysis of diffusion tensor imaging (DTI) images. This involves analyzing the brain's white matter tracts and their connectivity, providing insights into neural pathways and their integrity.
Conducting magnetic resonance spectroscopy (MRS) imaging and analyzing the obtained signals. This technique allows for the assessment of metabolic processes within the brain, aiding in the diagnosis and monitoring of various neurological conditions.
Preparation of three-dimensional metabolic maps of tumors. This involves utilizing imaging techniques to visualize and analyze the metabolic activity within tumors, providing valuable information for treatment planning and assessment.
Specialized imaging of epilepsy and subsequent analysis of the acquired images. This includes identifying epileptic foci and studying the brain's structural and functional abnormalities associated with epilepsy.
Performing volumetry, which involves measuring and quantifying the volume of specific brain structures or regions. This analysis contributes to understanding changes in brain anatomy and can assist in the diagnosis and monitoring of certain neurological disorders.
Imaging and analysis of perfusion images, which provide insights into the blood flow patterns within the brain. This information aids in the assessment of vascular abnormalities, such as ischemia or tumors, and can guide treatment decisions.